Postpartum Preeclampsia.
I have been posting a lot about #MaternalMentalHealth as it is #MentalHealthAwarenessMonth; but May is also #PreeclampsiaAwarenessMonth. Yesterday was #WorldPreeclampsiaDay, so I apologize for being a day late.
Perhaps some of you consider me an #oversharer these days, but I have decided transparency is the healthiest way for me to move forward in life. Some of you might not know about my preeclampsia journey, so here is my story.
Warning, I will be discussing details that may be traumatizing to some with birth trauma of their own.
I was re-hospitalized 4 days postpartum with severe postpartum preeclampsia. My blood pressure was 190/110, I was “leaking” protein, blood, and leukocytes. I had acute kidney injury with greatly impaired function. I had brain swelling as evidenced by hyperreflexia, clonus, vision changes, and a debilitating headache. I had referred right shoulder, rib, and chest pain from liver inflammation/distention as my liver was beginning to be affected and the worry was that I was heading towards HELLP syndrome. I was extremely swollen, short of breath (from the fluid build-up), had chest pain and tightness, nauseous, and was exhausted. I figured the fatigue, discomfort, and various complaints were normal for just being home with a newborn. I knew about preeclampsia, but my numbers were normal during pregnancy, so it was not even a thought in my mind. I didn’t have any of the risk factors, either. I had cardiomyopathy towards the end of pregnancy, but that had also regulated, so I wasn’t concerned. In fact, despite feeling so crummy, I also felt incredibly calm. It’s amazing what your mind does to protect you. Here I was dying, and my mind was like, “it’s cool, everything is fine, nothing is happening”. I would have never checked my blood pressure if Jessica hadn’t recommended it. And she only recommended it because I was shivering uncontrollably (which we now know is likely due to blood spilling), and we thought my blood pressure had bottomed out as it sometimes does with me. Imagine my surprise when it was so high! I took it several times, manually, and on the automatic cuff, before finally admitting to my family what it was. They all looked so panicked, and I just felt so calm and distant. They recommended the ER, I disagreed and said I would call the on-call OB. Ridiculous, right? The on-call OB said I absolutely needed to get in there. It was all such a blur and frenzy once there. I couldn’t understand the rush. I couldn’t understand the gravity of the doctor’s words, “we are going to admit you as you have severe preeclampsia and this is life-threatening”. I thought it comical when they were putting padding all over the bed because they were waiting for me to have a seizure at any moment. I really only recently came to understand that I likely wouldn’t be here writing this had we not gone to the hospital that night.
Postpartum preeclampsia is quite rare, affecting around only 600 women per year. While preeclampsia develops after 20 weeks of gestation, postpartum preeclampsia typically occurs within 48 hours of birth, but can develop up to 6 weeks after.
Risk factors for postpartum preeclampsia include: obesity, hypertension during pregnancy, family history of postpartum preeclampsia, being a mother under 20 or above 40, and/or having twins or multiple babies.
Risk factors for preeclampsia include: personal or family history of preeclampsia, chronic hypertension, first pregnancy, new paternity, very young or over 35 years of age, black women have the highest risk, obesity, multiples pregnancy, less than two years or more than 10 years between pregnancies, in vitro fertilization, and/or history of: migraines, diabetes, kidney disease, blood clots, lupus.
Preeclampsia is dangerous no matter when it occurs. But when it occurs during pregnancy, it is very dangerous to the baby as well. There is a huge racial disparity in treatment of pregnant women, and unfortunately the research continues to show that. Black women are most affected by this condition, and black women subsequently have the highest maternal mortality. We must fight not only for better research, early recognition, and treatment of preeclampsia, but also for equal treatment for all women.
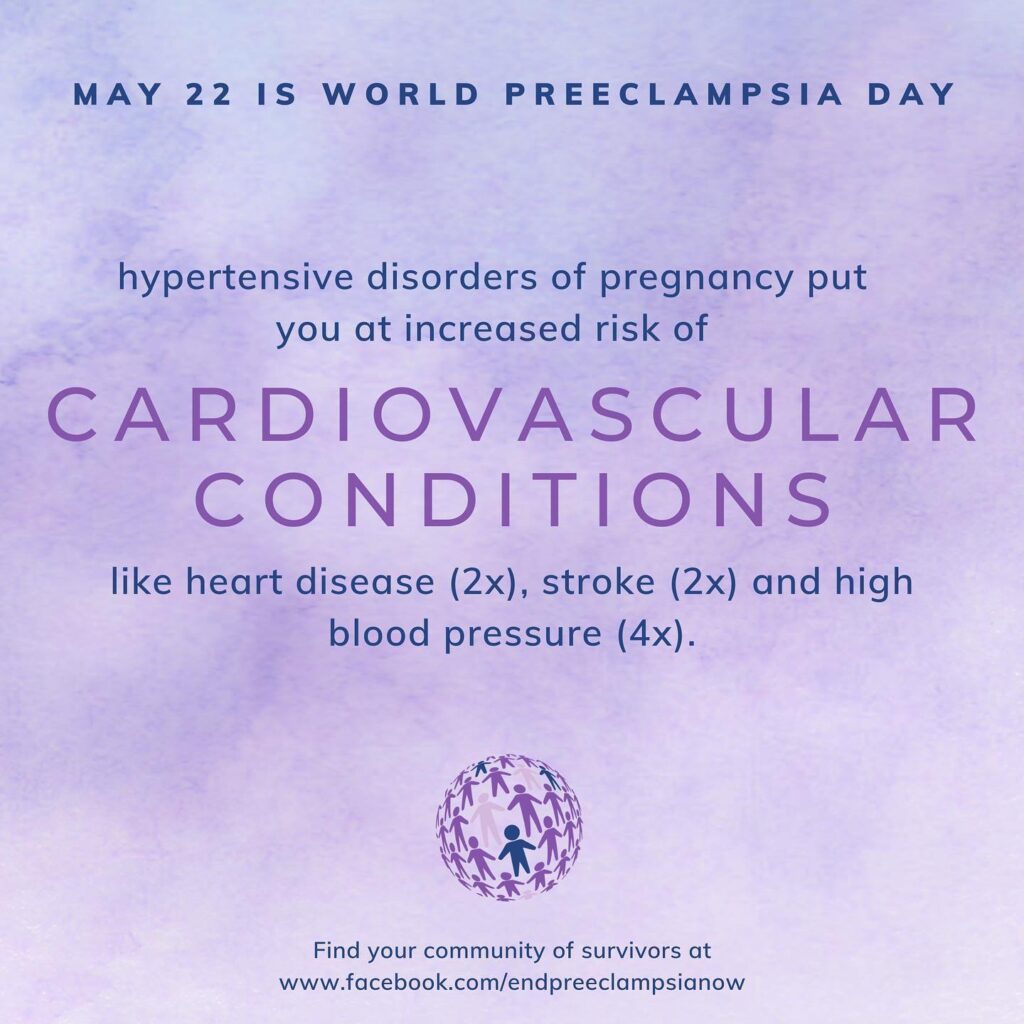
Preeclampsia, once treated, is “cured”. Unfortunately, there is sequalae (as shown in the graphic below), many of which, are still being discovered. So any Mamas that have suffered through preeclampsia while pregnant or during postpartum, please be diligent in your follow-ups.
One last thing I would like to discuss (yes, this is another novel), is the impact on mental health. Research shows that birth trauma greatly contributes to #perinatalmoodandanxietydisorders (you thought I would get through a post without discussing this, didn’t you?). Because this experience didn’t feel traumatic to me, I never thought I had a birth trauma. I felt so distant from what happened. Through treatment, some of my doctors kept mentioning that I seemed to be having a “trauma response”. I couldn’t understand what they meant. But my brain knew. Apparently when you brain perceives/knows your life to be in danger, it protects you from this trauma by separating itself from feeling what is going on, if you will. So I don’t feel any emotion connected to that situation… Yet. I will at some point. And I will work through it. It was traumatic. I can see that through an objective lens. The postpartum period has nearly killed me twice. That is heavy. I need to sit with it, experience it, and process it.
And no, we will not be having anymore children. Lol.
#postpartumpreeclampsia #preeclampsia #eclampsia #hellpsyndrome #womenshearthealth #cardiomyopathy #heartfailure #endpreeclampsia #mayispreeclampsiaawarenessmonth #worldpreeclampsiaday #onlychild #oneanddone #maternalmortality #maternalmentalhealth #maternalmentalhealthawarenessmonth #birthtrauma #ppptsd #ppd #ppa #maternalmentalhealthmatters #maternalhealthmatters #motherhoodisnotblackandwhite #equalaccesstocare #2020mom #momcongress #thebluedotproject
Resources:
EndPreeclampsia
Preeclampsia, Eclampsia & HELLP Syndrome Survivors
Preeclampsia Foundation
Action on Pre-eclampsia
Preeclampsia Initiative
Preeclampsia and Postpartum Preeclampsia Awareness